A preventable cancer: Why cervical cancer prevention week matters

Every year, cervical cancer week shines light on a disease that affects so many people with cervix’s worldwide, but is largely preventable.
Cervical cancer is when tumours form in the cervix (neck of the womb) due to abnormal cells growing uncontrollably, which causes HPV (persistent human papillomavirus). Screenings and vaccines help prevent, detect and treat the precancerous changes that can form into cancer. According to NHS England South East, ‘Cervical cancer causes around 685 deaths in England each year’.
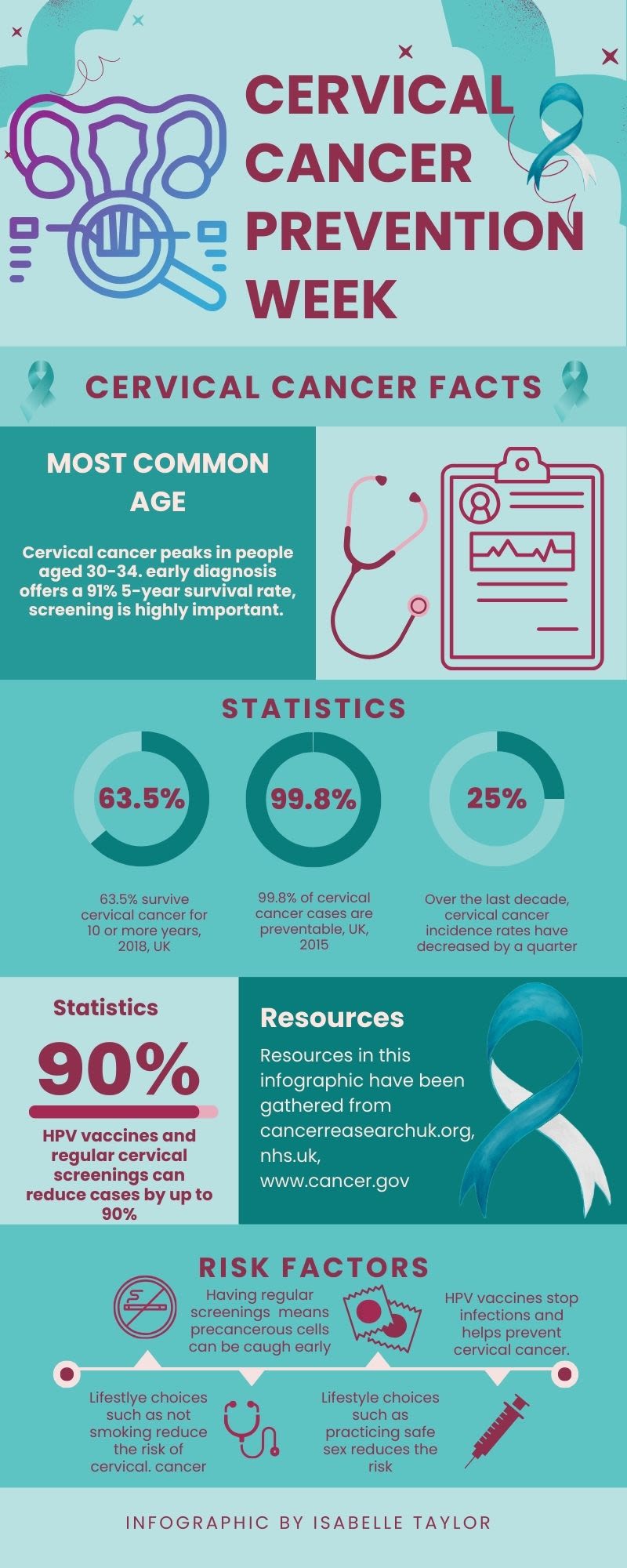
Cervical cancer graphic by Isabelle Taylor
Cervical cancer graphic by Isabelle Taylor
Often, in the early stages there are no symptoms, but in advanced cases, symptoms such as pelvic pain or unusual bleeding may occur.
The primary cause of cervical cancer is HPV infection. High-risk HPV types are transmitted through sexual contact. HPV causes abnormal cell changes in the cervix which if left untreated can turn into cancer; however, sometimes the infections can clear up on their own over time without any issues (but it’s always better to get checked).
Other risk factors and causes include, smoking, a weakened immune system and reproductive factors- such as using oral contraception and multiple births are higher risks.
Types of cervical cancer

There are two main types of cervical cancer: Adenocarcinoma, which can develop from glandular cells, and the second type is Squamous cell carcinoma, which develops from surface cells, and this is the most common type.
Squamous cell carcinoma is about 80-90% of cervical cancer cases, whilst adenocarcinoma takes up about 10-20%. The two other types- Adenosquamous carcinoma (a mix of both types) and small cell cancers (lymphomas and sarcomas) which are extremely rare and are often more aggressive. Lymphomas and sarcomas are treated in a different way to cervical cancers.
Infographic by Isabelle Taylor
Infographic by Isabelle Taylor
Prevention starts early
Health experts emphasise the importance of taking the necessary steps to prevent cervical cancer as its one of the most preventable forms of cancer. Having the HPV vaccination around the age of 12-13 (UK year 8) but, if this is missed it is available to those aged up to 25 for free on the NHS. Protection is better when given at an earlier age, before exposure to HPV.
The timing of the vaccination is important. The Centre of Disease Control and Prevention (CDC) recommends HPV vaccinations for girls and boys at 11 or 12 but can start from the age of 9. Depending on age, the vaccine is given in either 2 or 3 doses.
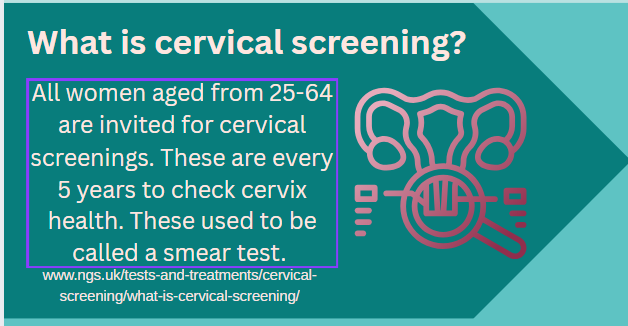
Cervical screenings are the next step in preventing cervical cancer. Jenny Greenfield a volunteer and trustee of UK Cervical Cancer Charity explains that although screenings may be scary or uncomfortable, we “have to be brave, take someone you trust, make sure you get that appointment and make sure you turn up”.
Infographic by Isabelle Taylor
Infographic by Isabelle Taylor
Screenings, formally known as ‘smear tests’ rates have dropped in recent years, from participation rates going from 80% in the 2000s to less than 70% by 2022 (NHS Digital). “We know there's a huge downfall in people taking up their smears/cervical screening, and a lot of this is because they’ve had the HPV immunisation, but people do need to attend their screenings,” said Jenny.
“A lot of people don’t come because they have maybe had a painful experience before, or its uncomfortable of they feel it's not necessary.”
Whilst it may be scary or uncomfortable, or life just gets in the way, Cervical screenings can save lives.
Why is talking about women’s health so Important?

Eleanor Davis, 22 is an ovarian cancer survivor. Diagnosed at just 18 years old, Eleanor didn't think she had any symptoms. Having gone to the doctors for another reason, the ‘bloating, suspected UTI and unexpected weight loss’ made sense when she was diagnosed at stage 1 in 2022.
Eleanor Davis | Photo credit- Isabelle Taylor
Eleanor Davis | Photo credit- Isabelle Taylor
In our interview, Eleanor spoke about women's healthcare as a whole. When asked about her experience prior to diagnosis, she described it as “a really great experience” given the consequences. But after was “left to my own devices” to find mental health support.
“Historically women’s health isn’t taken seriously”. We spoke about the need for more research, the need to have more offering of tests, as most young people (under the age of 25) aren’t offered cervical screenings as its only common in older women.
Cervical cancer prevention week not only focusses on raising awareness for cervical cancer, but all cancers that can occur in the womb.
Raising awareness
Cancer Matters Wessex focusses on not only raising awareness about Cervical cancer but also addressing healthcare more broadly. As it gets harder to get immediate GP appointments, DR Virginia Quiney, a GP who works with Cancer Matters Wessex spoke about the difficulty of getting appointments.
Dr. Virginia Quiney
Dr. Virginia Quiney
“I acknowledge that access to GPs is getting harder, and getting appointments is much more difficult, but practices do want to see people that need seeing and have health problems.”
Despite this, they are encouraging people to try and access the help they need. DR Quiney said to “not be scared of the consequences as it's always better to talk to someone about it and find out more about what's going on than just sit on your worries.”
Cancer Wessex matters are working hard to prevent cervical cancer, and the NHS hopes to eliminate it by 2040.
“So please do take up the opportunity to help reduce cervical cancer, whether that's through screening of taking up the vaccination if its available”
Support & resources
Information about going for cervical screenings can be found at We are the leading gynaecological cancers charity - The Eve Appeal
Welcome to Cancer Matters Wessex - Cancer Matters Wessex
Or call the number 0808 802 0019
Support for LGBTQ+ people and those with learning disabilities can be found at GOV.UK